A personal story of chronic sinus issues from ADVENT President and Founder, Madan Kandula, MD
We all have our reasons for not taking care of something like ongoing nasal problems and sinusitis—it’s inconvenient, it’s scary, it’s not bad enough yet—and I’m no different. But finally, in the spring of 2011, I reached the point where enough was enough. The doctor became the patient, and I had the very same kind of sinus surgery I perform to relieve sinus pain, congestion and chronic inflammation. I’m sharing my experience with you in the hope that it will help with your own decision-making, and to let you know that where sinus problems are concerned, I’ve been there.
My story began when I broke my nose in first grade. I was enjoying a snow day off from school going sledding with my saucer-style sled. Afterwards, I started making a snowman, with my sled sitting nearby on the snow. I took a giant step, turned, and set one of my boots down on the edge of the sled, which promptly sprang up and whacked me on the nose. Instant broken nose. Other than icing it, nothing was done about it at the time, but that incident set me on a path as far as my nose was concerned.
That was my first broken nose. The second happened when I was in college. It was another freak accident and, truth be told, sort of pitiful. I was messing around dancing, and smacked my nose on the shoulder of a friend. I heard it crack, saw it bleeding, and that really shut me down. Basically, I could hardly breathe through it, and ended up having surgery the summer of my junior year.
It was the old-school way of doing things where they re-broke the nose, repositioned it, and tried to straighten out the septum. I had my nose packed shut and was black and blue for a while afterwards. Once it healed I could get air through my nose again, and even though I sensed it wasn’t quite right, it was better than it had been. At least I didn’t have to sleep with my mouth open and I could get more restful sleep.
Despite the fact that my nose was “fixed,” I was still annoyed by congestion issues through med school, my residency and beyond. In fact, I believe that my choice of specialty was influenced in part by my own ongoing nasal problems. They turned into chronic sinus infections from 2004 on, when my wife and I began having children. The problems would usually start in fall and run through spring. They wouldn’t put me in bed, and I would end up fighting my way through, eventually giving in to taking antibiotics which would knock the infections down some. Remember, this is on top of my year-round congestion issues.
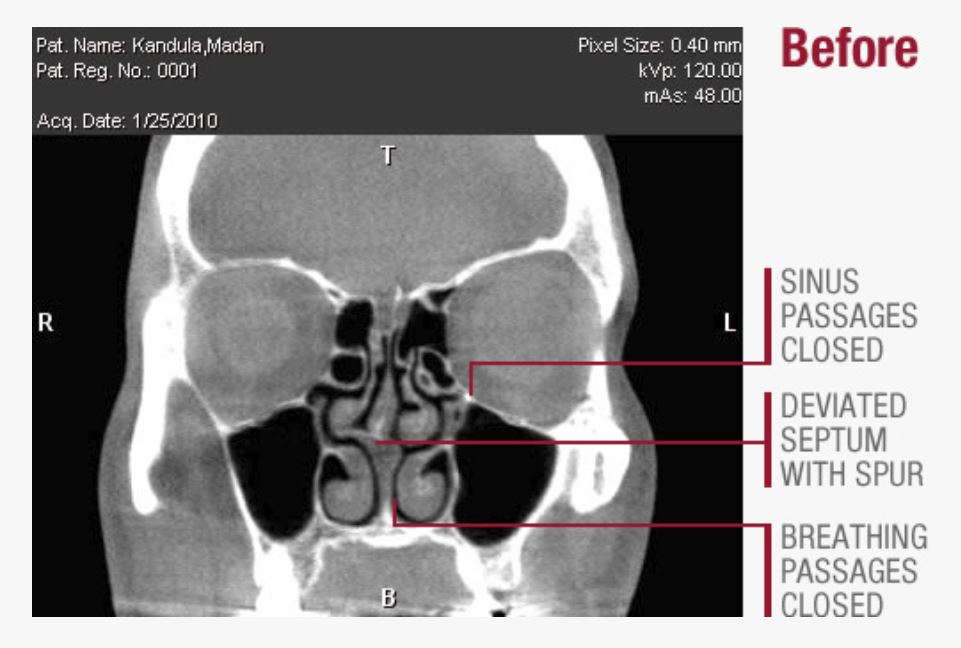
Then came the day we installed our in-office CT scanner. The Mini-CAT produces a digital image of the sinuses, which I can review with patients conveniently during their office visit. I volunteered myself as a test subject during training. Very revealing! For the first time I could see everything that was wrong: my septum was still bent in a major way, a bone spur was sticking into the side of my nose, there were blockages still, and the sinus passages were narrowed with some inflammation. I could clearly picture why I was having problems.
So I said to myself, now that I see it, if this were my patient, wouldn’t I recommend going ahead and getting it corrected? The other factor I was weighing is that I had dealt with migraine headaches since med school; they would really lay me down flat. The bone spur I saw in my scan is the kind of thing we look for with patients who have headaches, since it can be a trigger point for the nerve fibers that get irritated and spark a migraine. I wondered if that was contributing to mine.
Once it was evident I needed sinus surgery, I faced the same question as every patient: how do you find the right doctor? I had two criteria the surgeon needed to meet: Number one: someone who shared my mindset about utilizing the latest, state-of-the-art surgical approaches; and number two: someone with good hands! I ended up doing something that will sound very familiar to many of you. I asked around. I talked to other medical professionals, and especially valued the opinions of others who had seen surgeons operate and would recommend them to a friend or family member.
Eventually I found a surgeon in Chicago whose philosophical approach was very similar to mine, who was recently trained and who performed balloon sinuplasty. I also wanted a surgeon who was doing a lot of procedures, because that experience keeps your skills honed and makes you better and better.
The key test was showing him my scans (without telling him what I would do), and listening to his recommendation. When it was evident we were on the same page, I was very confident in going ahead with the surgery. Basically, the surgery I had was like a list of what I do for patients: straighten the septum; shrink the turbinates; enlarge the sinus passages in the cheek and between the eyes, using balloon sinuplasty on the sinuses in the forehead. The surgeon, also, removed my tonsils, which were diseased and causing chronic sore throats.

What was my recovery like? I was surprised—it was annoying (my throat was sore and my nose was stuffy), but I was able to manage and never took prescription pain medications. I didn’t have any packing in my nose (that’s not done anymore with advanced procedures), but had planned to take a week off and tried to lay low.
I was back at work the next week. Now, the further away from the procedure I get, the more significant the changes are. Prior to surgery, congestion was always there; some nights I could breathe decently, most nights not. When I lie down now, my nose is working fine. I have had my share of colds since surgery that, in the past, would have led to a sinus infection and the need for antibiotics. Nowadays, they came and go like they’re supposed to without complications. As for migraines, I haven’t had any. Bottom line, things played out exactly as I thought they would.
Could I have put up with sinus problems the rest of my life, the way many people do? Yes… but I knew that with today’s advancements, now was the time. Sinus surgery has gotten dramatically better the last 10 years or so—more targeted, more efficient, with less trauma than in the past.
The sinus issues I had are very common problems. Sadly, too many people are not aware of their options, or they’ve been told there’s nothing that can be done. They accept these conclusions without benefit of a sinus scan, like I finally had, which is the only way of telling the full story.
I see my role as giving patients choices, presenting the various scenarios and likely outcomes—these are the things we can do. Sinus problems won’t do you in, but they are quality of life issues. I hope that my story encourages others to seek out their options and not just continue to put up with sinus problems. I believe so strongly that today’s advanced procedures can restore quality of life that I was willing to undergo them myself.
__________
Since sinus surgery, Dr. Madan Kandula decided to undergo in-office balloon sinuplasty and turbinate reduction to help maximize his nasal breathing. Watch and read about his personal experience of those two simple, in-office procedures here.

